Blog
How to prevent medication errors in pharmacy
There’s an estimated 237 million medication errors a year in England alone. This causes between 712 and 1,708 deaths to patients.
While there is a small proportion of medication errors that can cause harm to your patient, you want to ensure you have done everything you can to reduce medication errors.
We provide a guide on lots of things you can do to give you peace of mind and reduce medication errors. One activity alone can detect 89% of medication errors before they occur.
What is a medication error in pharmacy?
A medication error is classed as a Patient Safety Incident (PSI) as it can cause harm to your patient.
It’s when there’s an error in the process of prescribing, preparing, dispensing, administering, monitoring or providing advice on medicines.
There are two categories of medication errors; errors of commissions or errors of omission.
Errors of commissions are mistakes such as giving the wrong dose of medication.
An error of omission is for example, when you fail to monitor or if you miss a dose.
Effects of medication errors
The majority, 72% of medication errors, will cause little or no harm to patients but there is 2% potential to cause severe harm. While the chances are low of causing significant harm to a patient, you do not want this to happen, and you do not want to doubt yourself and be distressed wondering if you have made a mistake.
For the small percentage where things go wrong, there could be harm such as developing a new condition like a rash or a drug interaction with other drugs. It can also lead to an increase in hospital admissions.
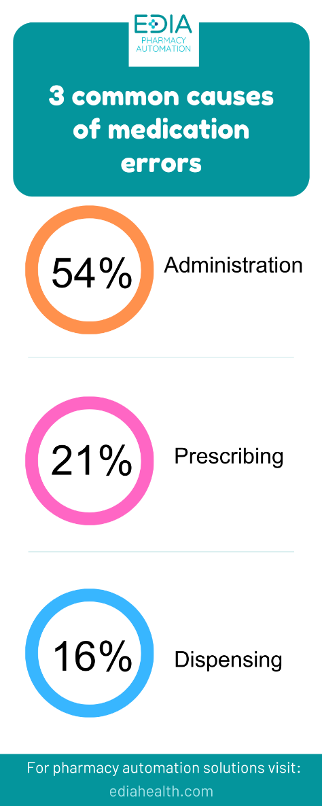
What are the three common causes of medication errors?
There are 3 types of medication errors which are most common:
- 54% medication administration
- 21% prescribing
- 16% dispensing
The most common drugs involved in medication errors include:
- non-steroidal anti-inflammatory drugs (NSAIDs)
- antiplatelets
- antiepileptics
- hypoglycaemics
- diuretics
- inhaled corticosteroids
- cardiac glycosides.
Medication error guidelines
It is important to follow guidelines to prevent medication errors and also when you realise there has been an error.
Patient Safety Professional Standards set out what is good practice and a framework for pharmacists across all service providers to follow as a medication error procedure.
Reflect
Reflect on existing knowledge and understand safety culture and systems to enable you to notice gaps regarding patient safety incidents. Improve on having safe and effective person-centred care and be responsive when a PSI occurs.
Review
Review all PSIs in a timely manner and identify any contributing factors, manage risk, and support safety interventions and learning.
Record and report
Record and report incidences in a timely manner and monitor and identify issues that need escalated to enable learning.
Act
Take the necessary action in a timely manner to improve quality of practice or systems of care and minimise contributory factors.
Share learning
Share your learning from any patient safety incidents with individuals and organisations and promote a learning culture to minimise future risks.
Evaluate
Regularly review systems, interventions and changes made to practice and assess outcomes of mitigating or preventing future risks and PSIs.
How can pharmacists reduce medication errors?
There are lots of things you can do to reduce the risk of medication errors. Not only can they help to reduce harm to patients, but they can give you peace of mind that you’ve done everything correctly. You don’t have to go home at the end of the day and wonder if you’ve made a mistake with a particular patient and spoil the time you do have away from work.

The 5 R’s of medication management
The 5 rights or 5 R’s act as a checklist for you when carrying out your role dispensing medication and help to ensure safe medication practice. They are:
- Right person
- Right medicine
- Right route
- Right dose
- Right time
Check and read back
Pharmacies are busy places, and it can be easy to fill in a prescription and not think twice about it.
But make sure to double-check what you’re doing and if possible, get someone to read it back to you.
Document everything
When you document everything, you can be reassured you have done everything correctly.
Simply by documenting it can make you take a minute to ensure it’s correct.

Storage
Having an organized workplace can help to reduce medication errors and save you time.
Make sure your workstation is tidy, the lighting is adequate, and you have enough counter space. Don’t store drugs that look alike together and have labels facing forwards to easily see what they are when you’re in a hurry.
Regularly check for any expired medication and carry out safety audits to keep on top of things.
Create culture of safety
Pharmacies are under a lot of pressure which can make it hard to find time to ensure everything runs smoothly. You may feel because members of staff or patients are waiting on you, that you need to rush.
Prioritise a culture of safety in your pharmacy. Communicate to staff and patients that because you prioritise safety, things may take longer but it is something you won’t take any shortcuts with.
When this kind of culture is embedded in your workplace, it allows staff to feel able to take time to ensure things are correct and to report errors if they should occur.
You can even carry out medication management training to instill it into your workforce.
Minimise distractions
Talking to people at the same time as preparing medication or doing other tasks can cause mistakes.
A high workload, interruptions, distractions, and inadequate lighting were shown to increase the occurrence of dispensing errors.
Since we know statistically these areas are likely to cause mistakes, ensure they are not an issue in your workplace.
Of course, a high workload isn’t easy to resolve but let other members of staff know not to ask you anything when you are dispensing.
Take lunch
Yes, it’s difficult to find time for a break or lunch when you have a heavy workload. You might have people asking you questions or you’re running behind. But having a break means it’s less likely you will be tired and fed up and make medication errors.
Just like creating a culture of safety, make sure members of staff know that lunch means no work.
Don’t use abbreviations
Using abbreviations is common in the medical industry but they can cause misunderstandings which lead to PSIs.
Common abbreviations include QD (once daily) and QID (4 times a day). Medication names can also be abbreviated and cause problems such as ‘AZT’ which can confuse ziovudine and azathioprine.
It’s not only abbreviations but zeros or decimal points can lead to misinterpretation and should be avoided or made clear.
Beware similar drugs
Drugs with similar names can also cause confusion, especially when it’s in a DRs handwriting. Drugs can either be orthographic which means they look like other drugs or phonological which means they sound like other drugs.
For example, atenolol and amlodipine can be confused.
Patient counselling
Simply talking with your patient can significantly reduce medication errors. Through patient counselling, 89% of medication errors were detected and corrected.
It’s not easy to find the time to speak to patients, but especially if it’s a new medication or not a routine script, then it could be helpful to speak to the patient.
Invest in automation
Investing in automation can reduce medication errors. While pharmacy automation machines still need to be overseen, they don’t get tired or distracted. Not only can they reduce medication errors, but they can save you time and give you peace of mind.
Automated and robotic dispensing systems along with other tech have contributed to a significant reduction in medication errors and patient harms. A systematic review of the effectiveness of these systems showed a 37% reduction in medication errors.
The review also showed an increase in productivity and reduced patient waiting and prescription filling time.
Not only does pharmacy automation help you, but it keeps your patients safe and provides better service.
You can choose from pharmacy vending machines, blister packing or pouch packing machines or medication checkers.
There’s a variety of choices that can help you save time and reduce medication errors.

Medication errors can be reduced. A small percentage of these errors will actually cause harm, but you don’t want to be the cause of this. Especially not when it can be prevented.
Understanding the most common types of medication errors and how they occur can make us more aware of these factors and prevent mistakes.
As a pharmacist, there are lots of ways to reduce medication mistakes.
Pharmacy automation can significantly help with this.
Edia provides a range of pharmacy automation machines that can improve your workflow and safety in your pharmacy.
Chat with us today about investing in pharmacy automation for your pharmacy.
Save time and resource
Automating prescription collections allows pharmacy staff to spend less time retrieving dispensed prescriptions and reduce patient waiting times.
Increase your market share
Get ahead of the curve and attract new patients by being the first in your area to offer 24/7 prescription collection
